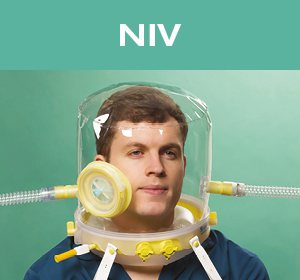
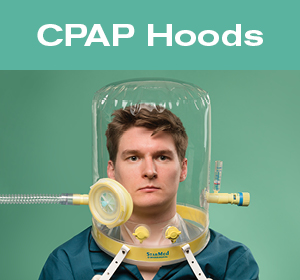
The StarMed range of respiratory hoods has been designed for both non-invasive ventilation (NIV) and CPAP therapy, providing an alternative patient interface to traditional masks.
The use of the hood interface helps to overcome many of the issues experienced with both endotracheal intubation and face mask use. It has been associated with increased patient comfort and improved NIV outcome, leading to reduced ventilation time and ICU length of stay.
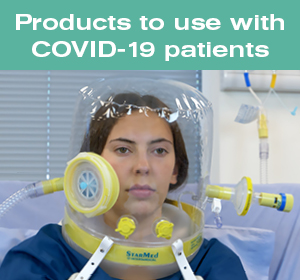
Beside the clinical advantages of the respiratory hoods for treating respiratory diseases, owing to the semi-closed environment design and the virtually leak-free seal, the StarMed interface has been identified as an optimal tool for reducing the risk of cross infection.
Benefits for the patient
Patient comfort - no pressure from the rigid plastic shell of the mask on the patient’s face and no headgear to tighten.
Airtight seal - the soft elastic membrane creates a perfect seal adhering to the patient’s torso. This improves patient comfort, preventing irritation to the eyes and ventilator asynchrony.
Smooth ventilation support - the whole environment is pressurised instead of just the airways.
Minimised claustrophobia - the sensation of claustrophobia is very rare, as the hood removes the discomfort, pain and the sense of suffocation associated with ventilator asynchrony.
Interaction possible - the patient can speak, listen, drink and wear glasses whilst being ventilated.
Benefits to the care giver
Easy hood positioning - once the patient’s head is in the hood the collar seals around the neck and remains airtight in semi-recumbent, supine or prone patient’s positioning.
Semi-closed environment - all expired gas from the patient is evacuated from the internal volume through the expiratory limb of the hood, which can be fitted with a breathing filter.
The hood is available in six adult sizes - allowing for the correct size to be easily selected, with the sealing membrane providing a level of tolerance within the size range.
Reduced nursing time - the hood does not need to be constantly repositioned if the patient moves as a good seal is maintained by the lower collar around the patient’s neck.
Easier management of the patient - when the patient drinks or expectorates they can easily be accessed via the port, with the hood staying in position, meaning only short disruption to therapy. A mask needs to be completely removed and then fully repositioned.
The CaStar Up - can be opened, quickly and easily by one operator, providing full access to the patient. The lower ring of the hood can stay in position for quick reconnection.
If the patient vomits - any gastric content will move away from the airway avoiding the risk of aspiration.

Resulting in improved therapy
Prolonged NIV application - as the hood is comfortable, it is well tolerated for long periods of ventilation and no need to relieve the patient from mask pressure every few hours. Clinical evidence shows average ventilation tolerance periods are longer with the hood than a mask. (1, 2, 3, 4)
Reduced NIV failure and intubation rate - the most frequent cause of NIV failure, leading to invasive ventilation, is patient discomfort, which is very rare in the hood. (2, 5, 6, 7, 8, 18)
Reduced risk of cross infection - owing to the semi-closed environment design and leak-free seal, the hood can help reducing the spread of expired particles from infective patients while noninvasive respiratory support is provided. (20, 21, 22)
Suitable for all types of patient and positioning - the hood can be used with a wide variety of adult and paediatric patients regardless of face shape, trauma, edentulism or beards. Hood ventiation in prone position is also described in clinical literature. (9, 10, 11, 25, 26)
Lower levels of sedation - patients using NIV masks often have to be sedated to prolong the compliance with the mask interface, whereas the hood requires lower levels of sedation. (12, 13)
Nebulised drug delivery and catheter access - drug delivery can be performed via an accessory during hood therapy without discontinuing ventilatory support. Sealed ports ensure there is no discomfort to the patient while using NG tubes or sensors.
Reduces total ventilation time and ICU length of stay - due to successful NIV outcome and uninterrupted therapy. (5, 7, 12, 14, 17, 18)
Improved NIV success and reduced costs - reduced ICU length of stay and the reduced need for sedation lead to cost savings. (13, 15, 18, 19)
Highly efficient interface for CPAP - the large internal volume can provide an optimal CPAP level, with a minimal evidence of pressure swings. (15, 16)
Allows respiratory support outside of the ICU - clinical studies describe the safe implementation of CPAP in medical wards to prevent ICU admission of some patients cathegories or to compensate for the lack of ICU beds. (14, 15, 23, 24)